Lesson 1: ECG Basics
- Tooba Alwani
- Feb 27
- 2 min read
Updated: Mar 27
Summary of Learning Points
The general approach to every ECG: Start with rate and rhythm. Then evaluate P-waves, PR intervals, Axis and QRS complex, QT interval, and lastly look for any Q waves and ST changes.
Rate can be identified by the box method (counting boxes between RR intervals) or counting the total number of complexes in the rhythm strip and multiplying by 6.
Rhythm: Identify if your rhythm is regular or irregular and narrow or wide complex. Differentiate between atrial (is it sinus?) and ventricular rhythm.
P waves: look in lead II and V1. Tall p-wave >2.5mm is RA problem, P-wave with a double hump in lead II or negative component in V1 is an LA problem
PR interval should be between 3 little boxes to 1 big box (0.12 to 0.2 seconds)
Axis: Always check lead I, II and aVF.
When sinus rhythm is present with intact AV conduction wide QRS >3 little boxes (120 ms) suggests a bundle branch morphology. Check leads V1, V6 and I to identify if it’s R or L!
Cornell criteria is the most sensitive criteria for LVH, combine the product of the S wave in V3 + R wave aVL.
Normal QT interval is less than 500 ms. Normally QT interval is less than half the R-R interval.
To identify ST changes always compare to TP segment and assess shape (concave up, down or flat)
Pathological Q waves are wider and deeper than benign Q waves and indicate infarcted myocardium
You can consistently see T wave inversions in aVR and V1 and often find T wave inversions in lead III and V2.
Peaked T waves are often seen in hyperkalemia, differential also includes acute ischemia.
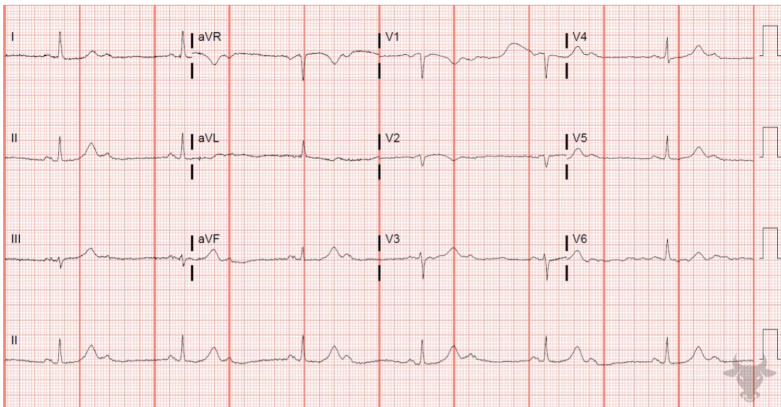
Practice ECG
Answer
Rate: ~ 150BPM (ventricular), atrial rate 300
Rhythm: Aflutter 2:1
P waves: None, flutter waves
PR interval: N/a
Axis: Left axis deviation (negative in II, positive in I)
QRS: Narrow, meets LVH criteria (sum of S wave in V3 + R wave in avL >28mm)
ST/T changes: Non-specific in distal precordial and lateral leads
Q waves: Inferior leads
QT: <500ms
Interpretation: Aflutter with 2:1 block, LVH with associated non-specific ST/T changes, possible prior inferior wall MI